An Effectiveness of RNA interference therapies in reducing urine and plasma oxalate levels among patients with primary hyperoxaluria- A systematic review
RNA interference therapies in primary hyperoxaluria- A systematic review
DOI:
https://doi.org/10.53778/pjkd93312Keywords:
primary hyperoxaluria, Lumasiran, nedosiran, RNA interfernce therapies, kidney stones, anemia, End stage kidney diseaseAbstract
Background:
Primary hyperoxaluria is a rare genetic disorder of hepatic oxalate over production. Standard of care was largely supportive with hyperhydration, urinary alkalinization and pyridoxine. RNA interference therapies have recently shown promising results.
Material and Methods:
The systematic review was prospectively registered with PROSPERO and followed PRISMA guidelines. Pubmed, EMBASE and CENTRAL were searched from January 1974 to July 2024 for randomized controlled trials and single arm intervention studies on use of RNAi therapies in primary hyperoxaluria.
Results:
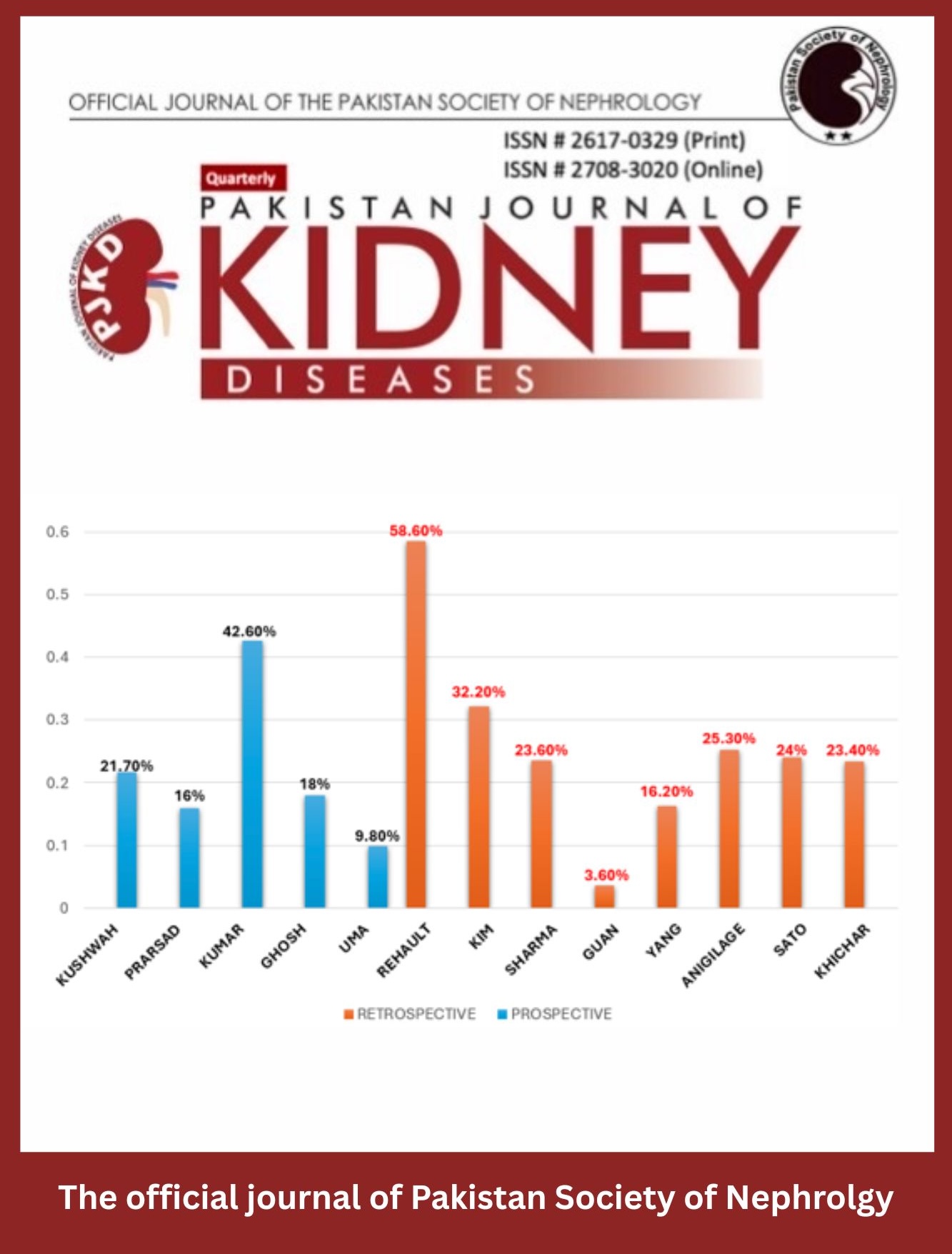
We found 127 records across the databases, with 12 of them included in the final analysis. A total of 140 patients were enrolled in Lumasiran (9 trials) and Nedosiran (3 trials). Most studies demonstrated a significant reduction in the oxalate burden. Injection site reaction was the most common adverse event with a largely acceptable safety profile. Quality of studies assessed through ROB-2 and ROBINS-I showed a low risk of bias.
Conclusion:
This systematic review emphasizes the effectiveness and safety of RNA interference therapies, Lumasiran and Nedosiran, in treating primary hyperoxaluria by lowering urinary and plasma oxalate levels.
References
Mandrile G, Beck B, Acquaviva C, Rumsby G, Deesker L, Garrelfs S, Gupta A, Bacchetta J, Groothoff J, OxalEurope Consortium/Erknet Guideline Workgroup On Hyperoxaluria. Genetic assessment in primary hyperoxaluria: why it matters. Pediatric Nephrology. 2023 Mar;38(3):625-34. https://doi.org/10.1007/s00467-022-05613-2
Fargue S, Acquaviva Bourdain C. Primary hyperoxaluria type 1: pathophysiology and genetics. Clinical Kidney Journal. 2022 May;15(Supplement_1):i4-8. https://doi.org/10.1093/ckj/sfab217
Gang X, Liu F, Mao J. Lumasiran for primary hyperoxaluria type 1: What we have learned?. Frontiers in Pediatrics. 2023 Jan 10;10:1052625. https://doi.org/10.3389/fped.2022.1052625
Chen T, Qian B, Zou J, Luo P, Zou J, Li W, Chen Q, Zheng L. Oxalate as a potent promoter of kidney stone formation. Frontiers in Medicine. 2023 Jun 5;10:1159616. https://doi.org/10.3389/fmed.2023.1159616
Bhasin B, Ürekli HM, Atta MG. Primary and secondary hyperoxaluria: Understanding the enigma. World journal of nephrology. 2015 May 5;4(2):235. https://doi.org/10.5527/wjn.v4.i2.235
Hashmi S, Abid A, Sultan S, Shekhani SS, Lanewala AA, Zafar MN. Primary hyperoxaluria and genetic linkages: an insight into the disease burden from Pakistan. Urolithiasis. 2022 Aug;50(4):439-45. https://doi.org/10.1007/s00240-022-01338-x
Demoulin N, Aydin S, Gillion V, Morelle J, Jadoul M. Pathophysiology and management of hyperoxaluria and oxalate nephropathy: a review. American Journal of Kidney Diseases. 2022 May 1;79(5):717-27. https://doi.org/10.1053/j.ajkd.2021.07.018
Somers MJ. Primary Hyperoxaluria: A Need for New Perspectives in an Era of New Therapies. American Journal of Kidney Diseases. 2023 Feb 1;81(2):131-3. https://doi.org/10.1053/j.ajkd.2022.08.005
Fargue S, Rumsby G, Danpure CJ. Multiple mechanisms of action of pyridoxine in primary hyperoxaluria type 1. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease. 2013 Oct 1;1832(10):1776-83. https://doi.org/10.1016/j.bbadis.2013.04.010
Devresse A, Cochat P, Godefroid N, Kanaan N. Transplantation for primary hyperoxaluria type 1: designing new strategies in the era of promising therapeutic perspectives. Kidney international reports. 2020 Dec 1;5(12):2136-45. https://doi.org/10.1016/j.ekir.2020.09.022
Forbes TA, Brown BD, Lai C. Therapeutic RNA interference: A novel approach to the treatment of primary hyperoxaluria. British Journal of Clinical Pharmacology. 2022 Jun;88(6):2525-38. https://doi.org/10.1111/bcp.14925
Scott LJ, Keam SJ. Lumasiran: first approval. Drugs. 2021 Feb;81:277-82. https://doi.org/10.1007/s40265-020-01463-0
Liu A, Zhao J, Shah M, Migliorati JM, Tawfik SM, Bahal R, Rasmussen TP, Manautou JE, Zhong XB. Nedosiran, a candidate siRNA drug for the treatment of primary hyperoxaluria: Design, development, and clinical studies. ACS Pharmacology & Translational Science. 2022 Sep 21;5(11):1007-16. https://doi.org/10.1021/acsptsci.2c00110
Sawyer K, Leahy S, Wood KD. Progress with RNA Interference for the Treatment of Primary Hyperoxaluria. BioDrugs. 2022 Jul;36(4):437-41. https://doi.org/10.1007/s40259-022-00539-5
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International journal of surgery. 2021 Apr 1;88:105906. https://doi.org/10.1016/j.ijsu.2021.105906
Frishberg Y, Deschênes G, Groothoff JW, Hulton SA, Magen D, Harambat J, van’t Hoff WG, Lorch U, Milliner DS, Lieske JC, Haslett P. Phase 1/2 study of lumasiran for treatment of primary hyperoxaluria type 1: a placebo-controlled randomized clinical trial. Clinical Journal of the American Society of Nephrology: CJASN. 2021 Jul;16(7):1025. https://doi.org/10.2215/cjn.14730920
Garrelfs SF, Frishberg Y, Hulton SA, Koren MJ, O’Riordan WD, Cochat P, Deschênes G, Shasha-Lavsky H, Saland JM, van’t Hoff WG, Fuster DG. Lumasiran, an RNAi therapeutic for primary hyperoxaluria type 1. New England journal of medicine. 2021 Apr 1;384(13):1216-26. https://doi.org/10.1056/nejmoa2021712
Hulton SA, Groothoff JW, Frishberg Y, Koren MJ, Overcash JS, Sellier-Leclerc AL, Shasha-Lavsky H, Saland JM, Hayes W, Magen D, Moochhala SH. Randomized clinical trial on the long-term efficacy and safety of lumasiran in patients with primary hyperoxaluria type 1. Kidney international reports. 2022 Mar 1;7(3):494-506. https://doi.org/10.1016/j.ekir.2021.12.001
Lieske J, Groothoff J, Frishberg Y, Sellier-Leclerc AL, Shasha-Lavsky H, Saland J, Hayes W, Magen D, Moochhala S, Coenen10 M, Simkova11 E. Efficacy and safety of lumasiran in patients with primary hyperoxaluria type 1: 24-month analysis of the ILLUMINATE-A trial. InAMERICAN JOURNAL OF KIDNEY DISEASES 2022 Apr 1 (Vol. 79, No. 4, pp. S1-S2). 1600 JOHN F KENNEDY BOULEVARD, STE 1800, PHILADELPHIA, PA 19103-2899 USA: WB SAUNDERS CO-ELSEVIER INC.
Saland J, Lieske J, Groothoff J, Frishberg Y, Shasha-Lavsky H, Magen D, Moochhala S, Simkova E, Coenen M, Hayes W, Hogan J. Efficacy and Safety of Lumasiran in Patients with Primary Hyperoxaluria Type 1: 36-Month Analysis of the ILLUMINATE-A Trial. InAMERICAN JOURNAL OF KIDNEY DISEASES 2023 Apr 1 (Vol. 81, No. 4, pp. S56-S57). 1600 JOHN F KENNEDY BOULEVARD, STE 1800, PHILADELPHIA, PA 19103-2899 USA: WB SAUNDERS CO-ELSEVIER INC.
Sas DJ, Magen D, Hayes W, Shasha-Lavsky H, Michael M, Schulte I, Sellier-Leclerc AL, Lu J, Seddighzadeh A, Habtemariam B, McGregor TL. Phase 3 trial of lumasiran for primary hyperoxaluria type 1: a new RNAi therapeutic in infants and young children. Genetics in Medicine. 2022 Mar 1;24(3):654-62. https://doi.org/10.1016/j.gim.2021.10.024
Hayes W, Sas DJ, Magen D, Shasha-Lavsky H, Michael M, Sellier-Leclerc AL, Hogan J, Ngo T, Sweetser MT, Gansner JM, McGregor TL. Efficacy and safety of lumasiran for infants and young children with primary hyperoxaluria type 1: 12-month analysis of the phase 3 ILLUMINATE-B trial. Pediatric Nephrology. 2023 Apr;38(4):1075-86. https://doi.org/10.1007/s00467-022-05684-1
Michael M, Groothoff JW, Shasha-Lavsky H, Lieske JC, Frishberg Y, Simkova E, Sellier-Leclerc AL, Devresse A, Guebre-Egziabher F, Bakkaloglu SA, Mourani C. Lumasiran for advanced primary hyperoxaluria type 1: phase 3 ILLUMINATE-C trial. American Journal of Kidney Diseases. 2023 Feb 1;81(2):145-55. https://doi.org/10.1053/j.ajkd.2022.05.012
Hoppe B, Koch A, Cochat P, Garrelfs SF, Baum MA, Groothoff JW, Lipkin G, Coenen M, Schalk G, Amrite A, McDougall D. Safety, pharmacodynamics, and exposure-response modeling results from a first-in-human phase 1 study of nedosiran (PHYOX1) in primary hyperoxaluria. Kidney international. 2022 Mar 1;101(3):626-34. https://doi.org/10.1016/j.kint.2021.08.015
Baum MA, Langman C, Cochat P, Lieske JC, Moochhala SH, Hamamoto S, Satoh H, Mourani C, Ariceta G, Torres A, Wolley M. PHYOX2: a pivotal randomized study of nedosiran in primary hyperoxaluria type 1 or 2. Kidney international. 2023 Jan 1;103(1):207-17. https://doi.org/10.1016/j.kint.2022.07.025
Goldfarb DS, Lieske JC, Groothoff J, Schalk G, Russell K, Yu S, Vrhnjak B. Nedosiran in primary hyperoxaluria subtype 3: results from a phase I, single-dose study (PHYOX4). Urolithiasis. 2023 Apr 28;51(1):80. https://doi.org/10.1007/s00240-023-01453-3
Singh P, Viehman JK, Mehta RA, Cogal AG, Hasadsri L, Oglesbee D, Olson JB, Seide BM, Sas DJ, Harris PC, Lieske JC. Clinical characterization of primary hyperoxaluria type 3 in comparison with types 1 and 2. Nephrology Dialysis Transplantation. 2022 May 22;37(5):869-75. https://doi.org/10.1093/ndt/gfab027
Hoppe B, Martin-Higueras C. Improving treatment options for primary hyperoxaluria. Drugs. 2022 Jul;82(10):1077-94. https://doi.org/10.1007/s40265-022-01735-x
Somers MJ. Primary hyperoxaluria: a need for new perspectives in an era of new therapies. American Journal of Kidney Diseases. 2023 Feb 1;81(2):131-3. https://doi.org/10.1053/j.ajkd.2022.08.005
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Pakistan Journal of Kidney Diseases

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.