Incidence of Catheter-Related Infections in Maintenance Hemodialysis Patients: A Critical Challenge in Balochistan, Pakistan
DOI:
https://doi.org/10.53778/pjkd93310Keywords:
Catheter-Related Infections, Hemodialysis, Central Venous Catheter, Diabetes Mellitus, Bloodstream Infection, Pakistan, Cross-Sectional StudyAbstract
Background: Catheter-related infections (CRIs) represent a critical complication in haemodialysis patients, particularly in resource-limited settings. This study investigated the incidence, risk factors, and predictors of CRIs among haemodialysis patients at Sandeman Provincial Hospital, Quetta, Balochistan, Pakistan.
Methods: A cross-sectional observational study was conducted from January 2023 to December 2024, enrolling 357 adult patients with end-stage renal disease undergoing maintenance haemodialysis via central venous catheters. Data were collected using structured questionnaires covering demographics, clinical parameters, catheter characteristics, and institutional factors. Statistical analyses included descriptive statistics, chi-square tests, Mann-Whitney U tests, logistic regression, and Kaplan-Meier survival analysis.
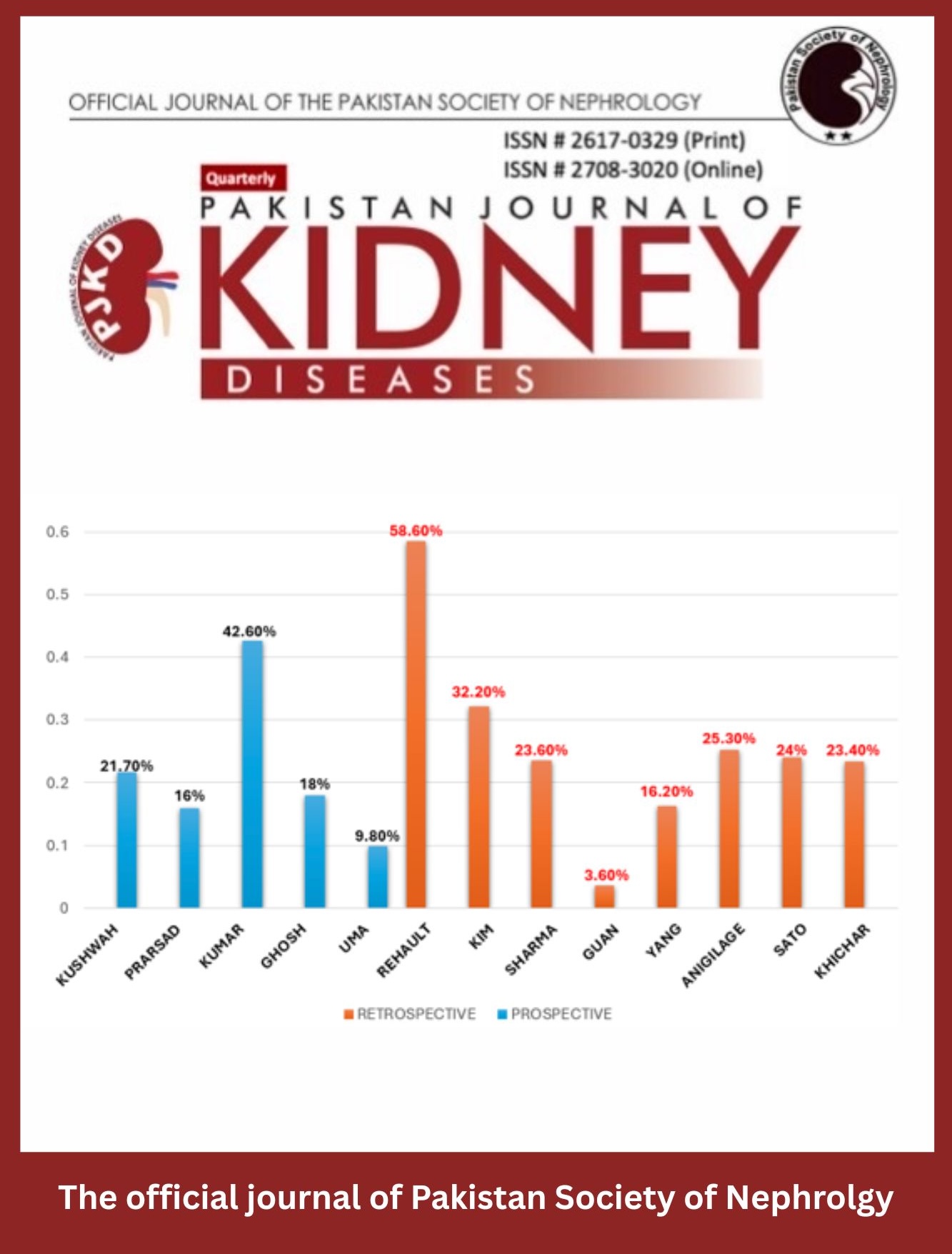
Results: The CRI incidence was exceptionally high at 82.1% (293/357 patients), with exit-site infections predominating (96.2%) and catheter-associated bloodstream infections accounting for 22.9%. Diabetes mellitus emerged as the strongest predictor (adjusted OR = 6.3, P < 0.001), followed by non-sterile gauze use (OR = 4.2) and hypertension (OR = 3.1). Femoral catheters were associated with higher bloodstream infection rates compared to subclavian access (P = 0.023). Critical institutional gaps included suboptimal hand hygiene compliance (73%), minimal staff training rates (2.2-10.9%), and zero utilization of antibiotic lock therapy.
Conclusions: CRI rates at this facility far exceed international benchmarks, driven by modifiable patient-specific, procedural, and institutional factors. Urgent implementation of evidence-based interventions including improved infection control protocols, staff training, and catheter care bundles is essential to reduce this preventable burden in Balochistan's vulnerable haemodialysis population.
References
Lodhi A, Sajjad A, Mehmood K, Lodhi A, Rizwan S, Ubaid A, et al. Profile and predictors of hepatitis and HIV infection in patients on hemodialysis of Quetta, Pakistan. Drug Discov Ther. 2019;13(5):274-9.
Nargus S. Assessment of Infection Control Practices in Bolan Medical Complex and Sandeman Provincial Hospital of Quetta, Balochistan, Pakistan. International Blood Research & Reviews. 2022.
Mahmood MH. Incidence of catheter-association bloodstream infection among hemodialysis patients at Erbil Teaching Hospital. Cell Mol Biol (Noisy-le-grand). 2024;70(10):174-81.
Nasiri E, Rafiei MH, Mortazavi Y, Tayebi P, Ghasemzadeh Bariki M. Causes and Risk Factors of Hemodialysis Catheter Infection in Dialysis Patients: A Prospective Study. Nephro-Urology Monthly. 2021.
Hajji M, Neji M, Agrebi S, Nessira SB, Hamida FB, Barbouch S, et al. Incidence and challenges in management of hemodialysis catheter-related infections. Sci Rep. 2022;12(1):20536.
Rashid S, Quershi M, Moon F, Qamar M, Danial K, Abid K. Frequency of Catheter Infections in Patients of Hemodialysis Despite Using Antibiotic Lock. Pakistan Journal of Health Sciences. 2022.
Bravo Thompson HA, Campos Herrera FA, Macías Ibiricu DA, Rodríguez Barrios SI, Vázquez Acevedo DI, Candanedo Gonzalez CA, et al. Factors Related to the Development of Infective Endocarditis in Hemodialysis Patients in a Third-Level Hospital in Panama. Cureus. 2024;16(1):e52385.
Andita HF, Abidin Z, Hamim N. EFFECTIVENESS OF DOUBLE LUMEN CATHETER WOUND CARE USING 0.9% NaCL, 7.5% CHLORHEXIDINE, 15% CETRIMIDE ON DOUBLE LUMEN CATHETER INFECTION IN REGULAR HEMODIALYSIS PATIENTS. Nurse and Health: Jurnal Keperawatan. 2024.
Khan AM, Khan MK, Zubair M, Khan S, Khalid U, Sultan K. Hemodialysis Catheter-Related Infections: Incidence in Temporary Catheters locked with Vancomycin and Heparin vs. Heparin-only. Journal of Pharmaceutical Research International. 2022.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4(10):e296.
Cevallos M, Egger M. STROBE (STrengthening the Reporting of Observational studies in Epidemiology). Guidelines for Reporting Health Research: A User's Manual2014. p. 169-79.
Ling ML, Apisarnthanarak A, Jaggi N, Harrington G, Morikane K, Thu LTA, et al. APSIC guide for prevention of central line associated bloodstream infections (CLABSI). Antimicrobial Resistance & Infection Control. 2016;5:1-9.
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Pakistan Journal of Kidney Diseases

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.